Robotic Low Anterior Resection with Diverting Loop Ileostomy for Locally Advanced Rectal Cancer
Abstract
This video demonstrates a robotic low anterior resection for locally advanced rectal cancer after neoadjuvant FOLFOX-based chemoradiation treatment. Low anterior resection is recommended for rectal tumors in which a 1-cm distal margin is achievable without sphincter encroachment. A key component of this operation is a complete mesorectal dissection, which is highlighted with the robotic technique. In this case, our patient had a 2.6-cm tumor located 6 cm above the anal verge, which was treated with eight cycles of FOLFOX followed by consolidative radiation therapy. A robotic low anterior resection was performed, and the final pathology revealed a complete pathologic response.
Case Overview
Background
Colorectal cancer is the third leading cause of cancer related deaths in the United States; however, improved overall survival in rectal cancer has been demonstrated with the addition of FOLFOX-based total neoadjuvant therapy. Although some patients will have a complete clinical response post-therapy, ongoing surveillance is recommended. Surgery, including low anterior resection (LAR) or abdominoperineal resection (APR), is recommended for all patients with residual disease or recurrence. A robotic approach to LAR for low-lying tumors above the sphincter complex provides unparalleled visualization of the mesorectum during oncologic resection. In this video, we demonstrate a robotic low anterior resection for a patient with locally advanced rectal cancer, who had been treated with neoadjuvant FOLFOX-based chemoradiation.
Focused History of the Patient
Our patient is an otherwise healthy 50-year-old female who presented in early November 2020 for screening colonoscopy. A moderately differentiated rectal adenocarcinoma with intact mismatch repair genes approximately 6–12 cm from the anal verge and occupying 30% of the luminal circumference was identified. The mass was felt about 6–7 cm from the anal verge during digital rectal examination. The patient was notably asymptomatic from this lesion.
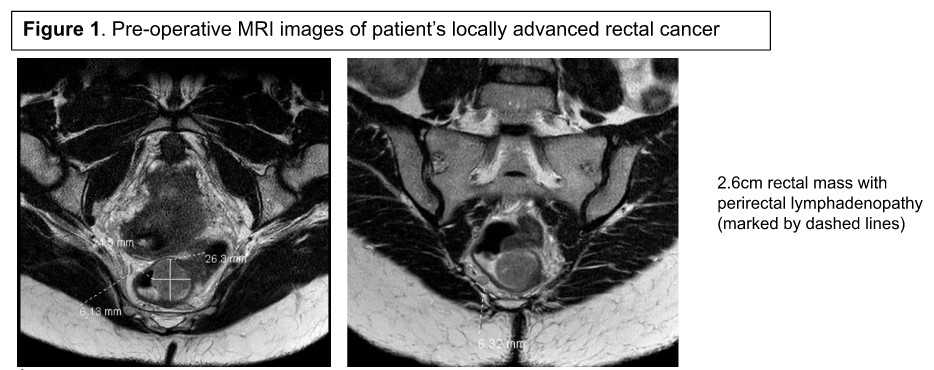
Staging work-up including axial imaging of the chest, abdomen, and pelvis was negative for distant or peritoneal metastases. In addition, an MRI was performed, which showed a semi-circumferential 2.6-cm rectal mass with borderline enlarged mesorectal lymph nodes consistent with cT3, cN1, cM0 (Stage IIIB) disease (Figure 1). Her carcinoembryonic antigen (CEA) level was 7.9 ng/mL.
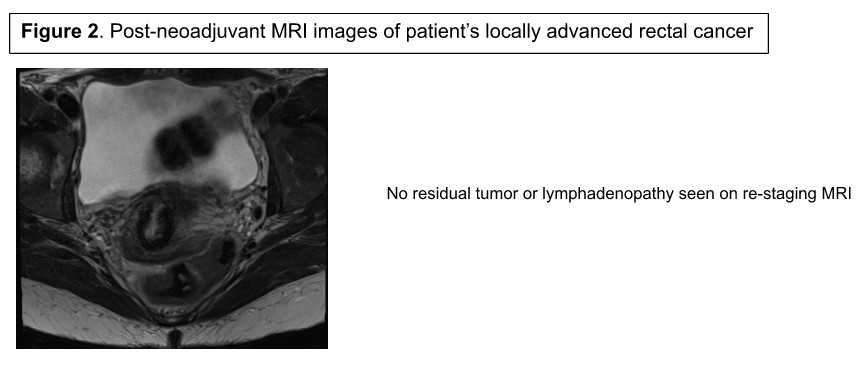
The patient was referred for neoadjuvant therapy, and eight cycles of FOLFOX-based chemoradiation were completed in July 2020. Re-staging MRI did not demonstrate residual tumor or perirectal adenopathy (Figure 2); however, a flexible sigmoidoscopy showed adenomatous tissue at the level of the tumor suggestive of residual disease. The risks and benefits of observation versus surgery were discussed in a multidisciplinary manner, and the patient agreed to proceed with robotic LAR. As with any LAR approach, a 1-cm margin and complete mesorectal excision sampling at least a minimum of 12 lymph nodes is necessary for adequate resection.
Discussion
The patient was brought to the operating room and positioned supine with arms abducted. The arms and torso were secured with a combination of bean bag and safety straps to prevent shifting with table repositioning. Port placement is planned prior to prepping and detailed in Figure 3.
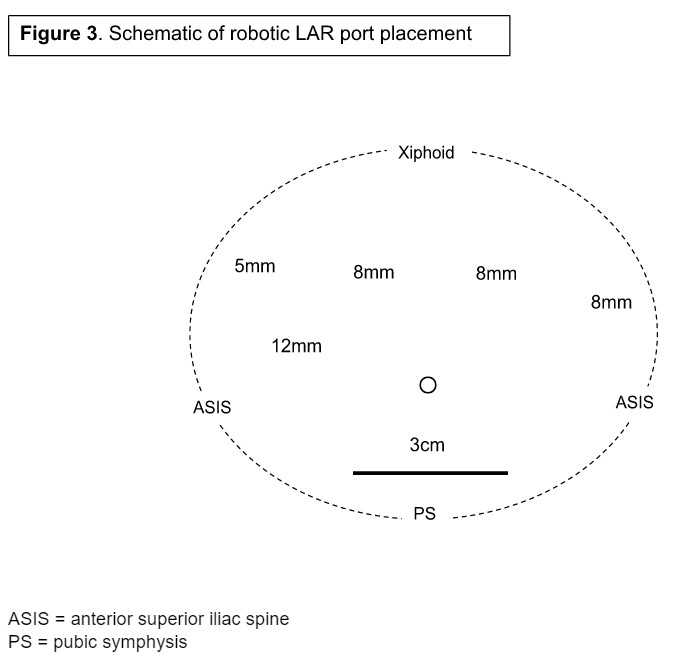
We began with a 3-cm Pfannenstiel incision about 2 fingerbreadths above the pubic symphysis. This incision served as both our initial camera port and specimen extraction site. An Alexis wound protector was inserted, and a 12-mm trocar was placed through the port. Pneumoperitoneum was established, and the abdomen was explored for occult metastatic disease. Additional 8-mm ports were placed under direct visualization in the right lower quadrant port, one handsbreadth medial to the anterior iliac spine as well as at equidistance points across the abdomen in the left epigastric region and left upper quadrant. A final 5-mm AirSeal working port was inserted in the lumbar region to triangulate between the rigtht lower quadrant and left epigastric ports. Note that if a diverting ostomy is planned, the right lower quadrant port site is often used. The DaVinci robot was then docked, and working instruments were inserted into the trocars. Note that the right lower port site was upsized to 12 mm and used as the camera port.
The patient was next positioned in slight Trendelenburg with the right side down to facilitate mobilization of intraabdominal contents. The omentum was swept cephalad to the transverse colon, and the small bowel was tucked in the right upper quadrant. Our dissection began in lateral-to-medial fashion by freeing the sigmoid colon from the pelvic brim and side wall. The white line of Toldt was incised to elevate the descending colon and its mesentery proximally to the level of the splenic flexure.
Once mobilized, we next identified the inferior mesenteric artery pedicle and developed a plane between the vessel and the retroperitoneum. This was extended laterally to our prior lateral-to-medial dissection. To avoid inadvertent injury, the ureter was clearly visualized during this portion of the dissection.
Next, we moved cephalad to complete the medial-to-lateral dissection by first incising the peritoneum just lateral to the ligament of Treitz. The inferior mesenteric vein was identified, encircled, and taken with an energy device. This portion of the medial dissection was extended beneath the transverse mesocolon and out laterally towards the splenic flexure. Overlying omental attachments and the gastrocolic ligament were incised to completely free the splenic flexure and ensure adequate colonic length for the colorectal anastomosis. Attention was then returned to the medial dissection, which was extended caudally towards the IMA root.
With the proximal portion of the dissection complete, we proceeded to dissect the proximal rectum away from the pelvic brim and sidewall with careful preservation of the hypogastric nerve plexus. This enabled our entry into the correct plane for elevating the entire mesorectum from the retroperitoneum. We completed rectal our dissection by incising of the peritoneal reflection circumferentially around the pouch of Douglas and further mobilizing the extraperitoneal rectum caudally. Flexible sigmoidoscopy was performed to ensure the dissection was below the residual tumor.
Next, two firings of the green load Endo-GIA stapler were then used to transect the dissected distal rectum. The colonic dissection was completed by ligating the IMA just distal to the left colic take-off. The colonic mesentery was divided up to the level of the proximal transection after ICG angiography confirmed adequate perfusion. The specimen was then exteriorized through the Pfannenstiel incision.
The proposed proximal transection site was cleared of any pericolic fat and sharply divided. An automatic purse string device was used to thread a Prolene suture around the colotomy. A 28-French EEA Covidien anvil was inserted into the lumen, prolene tied, and colon returned to the peritoneal cavity.
Pneumoperitoneum was then re-established, and the Covidien stapler was inserted through the anus. The spike was deployed posterior to the middle of the rectal staple line, and a Prolene purse string was placed around the spike. The anvil was joined to the end of the stapler and fired. A full-thickness, running V-lock suture was used to oversew the anastomosis. The flexible sigmoidoscope was inserted to examine the anastomosis and perform a leak test.
Because the tumor was within 7 cm of the anal verge and had been treated with neoadjuvant therapy, a temporary diverting loop ileostomy was prepared. A segment of ileum about 20 cm proximal to the ileocecal valve was identified and grasped. The skin around the right lower quadrant port site was excised, and the soft tissues were dissected down to the fascia. The fascia was incised in cruciate fashion, and the muscle fibers split. The selected segment of ileum was then brought through the aperture without difficulty. The stoma was matured in Turnbull-Brooke fashion with interrupted tripartite Vicryl sutures.
The patient tolerated the procedure and had an uneventful postoperative recovery. She was discharged home on postoperative day 3. Final pathology revealed a complete pathologic response with no residual tumor and 0/24 positive lymph nodes. She was seen in follow-up and continues to do well. Her ostomy will be reversed about 12 weeks from surgery.
Several prospective and retrospective reviews have considered factors associated with anastomotic leak in low anterior resections.1 In instances of low rectal tumors (<7 cm from the anal verge) and neoadjuvant chemoradiation, anastomotic leak rates are higher.1, 2 Temporary diversion with a loop ileostomy is therefore recommended in these instances.
In terms of the benefit of the robotic approach, a recent study demonstrated a higher rate of complete mesorectal dissection, and fewer nearly complete or incomplete dissections compared to laparoscopy.3 It is important to remember, however, that surgeon experience in different approaches should dictate the low anterior resection approach.
Equipment
No special equipment or implants.
Disclosures
Nothing to disclose.
Statement of Consent
The patient referred to in this video article has given their informed consent to be filmed and is aware that information and images will be published online.
Acknowledgments
None.
Citations
- Sciuto A, Merola G, De Palma GD, Sodo M, Pirozzi F, Bracale UM, Bracale U. Predictive factors for anastomotic leakage after laparoscopic colorectal surgery. World J Gastroenterol. 2018;24(21):2247-60. doi:10.3748/wjg.v24.i21.2247.
- Park JS, Choi GS, Kim SH, et al. Multicenter analysis of risk factors for anastomotic leakage after laparoscopic rectal cancer excision: the Korean laparoscopic colorectal surgery study group. Ann Surg. 2013;257(4):665-71. doi:10.1097/SLA.0b013e31827b8ed9.
- Baik SH, Kwon HY, Kim JS, Hur H, Sohn SK, Cho CH, Kim H. Robotic versus laparoscopic low anterior resection of rectal cancer: short-term outcome of a prospective comparative study. Ann Surg Oncol. 2009;16(6):1480-7. doi:10.1245/s10434-009-0435-3.


